From 1 November 2025, changes will be introduced to the Better Access to Psychiatrists, Psychologists and General Practitioners through the Medicare Benefits Schedule (MBS) initiative.
These changes, brought in by the Department of Health, Disability and Aged Care and designed to be consistent with recommendations from the Better Access Evaluation in 2022, are intended to:
- Improve equity of access to mental health supports and services.
- Support coordinated care between patients and their healthcare providers.
- Reduce administrative complexity for GPs and Prescribed Medical Practitioners by allowing greater flexibility through time-tiered general attendance MBS items for mental health treatment plan reviews, referrals, and consultations.
The updates aim to:
- Link mental health treatment plans, reviews, and referrals to a patient’s MyMedicare practice or usual medical practitioner.
- Integrate physical and mental health care by removing specific MBS items for mental health plan reviews and consultations, enabling use of general attendance items instead.
- Provide guidance material to support best-practice referral and review processes aligned with the Australian Government’s stepped care model.
For the specific details on what the changes are that impact you, including the PDFs and fact sheets, visit:
- MBS Online – Better Access changes from 1 November 2025
- RACGP - Better Access changes from 1 November 2025
Referral requirements under the Better Access Initiative
In addition to an eligible patient having a mental health diagnosis and a mental health treatment plan (MHTP), a patient must have a valid referral to receive Better Access mental health treatment services. The referral letter template (in addition to the template specifically used for Aboriginal and Torres Strait Islander patients) can be found here.
Mental health treatment services are generally provided in two courses of treatment per year (if required). Depending on the patient’s needs and following the initial course of individual treatment (involving up to 6 services on the initial referral), patient’s can return to their GP or PMP who will undertake a review of a patients MHTP and assess if their patient needs further treatment. These limits do not apply to group therapy services. Up to 10 group therapy services can be specified in a single referral. Patients may also receive a referral for a course of individual mental health treatment services and group therapy mental health treatment services at the same time.
When referring a patient for mental health treatment services under Better Access, services should be utilised for patients who require at least a moderate level of support. If a patient does require mental health treatment services under the Better Access initiative, GPs and PMPs should refer to explanatory note AN.15.6 which outlines the requirements when referring patients to MBS supported allied health services. In addition to the referral requirements set out in AN.15.6 , the following must be included on the referral for patients to received mental health treatment services:
- the patient's name, date of birth and address
- the patient's symptoms or diagnosis
- a list of any current medications
- the number of services the patient is being referred for
- a statement about whether the patient has had a Mental Health Treatment Plan or a Psychiatrist Assessment and Management Plan prepared
Specifying the number of services allowed per course of treatment ensures the allied health professional is managing the patient’s allocation within the annual limit, maintaining eligibility for Medicare benefits.
Further information on referral requirements for Better Access treatment services can be found at explanatory note MN.6.3.
Medicare Mental Health Check In media release which advises of the Provider identified to deliver National Early Intervention Service.
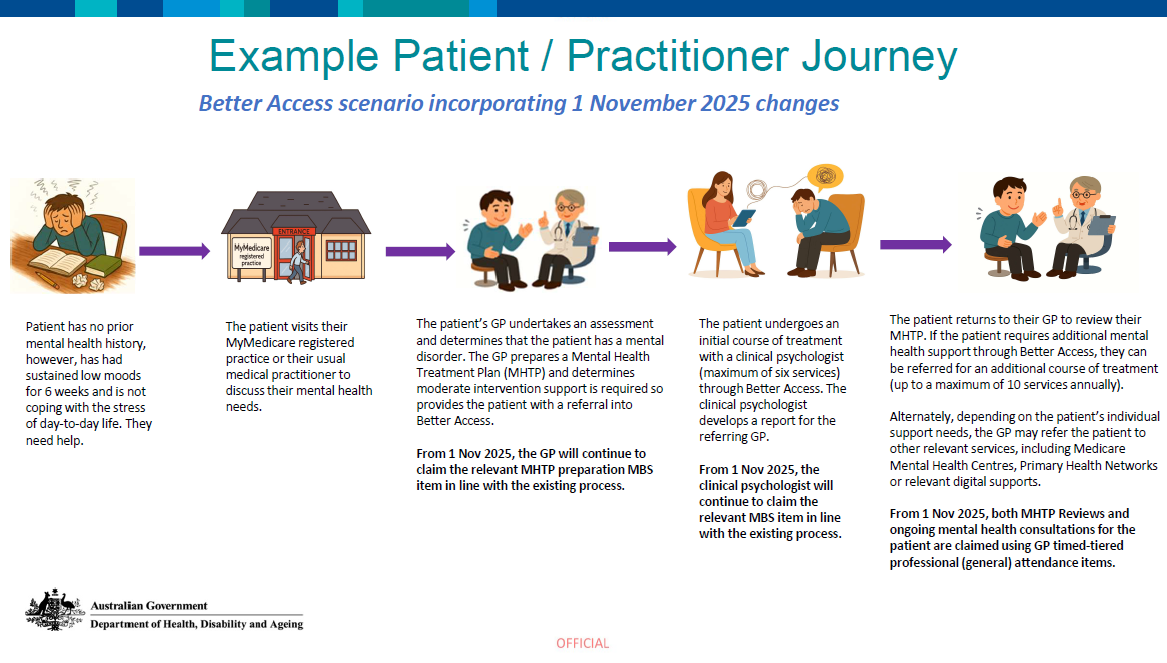
See below for an example patient journey scenario
A patient with no previous mental health disorder visits their GP for support. The GP conducts a mental health assessment and diagnoses a mental disorder. In this case, the GP determines the patient has at least moderate mental health support intervention needs and therefore deems it appropriate to prepare a Mental Health Treatment Plan and a referral to access Better Access services. The GP will continue to use existing MBS items to prepare the mental health treatment plan.
To claim a Medicare benefit a patient can EITHER see:
- a General Practitioner or Prescribed Medical Practitioner at their MyMedicare registered practice, or
- their usual medical practitioner (regardless of their MyMedicare registered status). This includes other GPs and PMPs who are employed at the patient’s usual medical practice location.
For a patient to be eligible for telehealth (video and phone) services for the preparation of a MHTP under Better Access, patients must have had at least 1 face-to-face appointment in the previous 12 months with a GP or PMP at their usual medical practice or meet any of the other exemptions to the established clinical relationship rule or are receiving their telehealth service from a GP or PMP at their MyMedicare regstered practice. Further information on telehealth requirements and exemptions is available at MBS Online - MBS Telehealth Services.
The GP provides the patient with an initial referral for up to 6 individual services with a clinical psychologist. As already mentioned, there are no changes to existing Better Access treating practitioner or allied health professional MBS items. The clinical psychologist will continue to use existing MBS items to deliver these mental health treatment services.
At the completion of the initial course of treatment, the clinical psychologist will provide a written report back to the referring GP, and includes the following information:
- assessments carried out on the patient,
- treatment provided, and
- recommendations on future management of the patient’s condition.
After the initial course of treatment, the patient returns to their referring GP. The GP reviews the Mental Health Treatment Plan and assesses the need for further services if required, in conjunction with the clinical psychologist’s report. A review of a patient’s mental health treatment plan should not occur more than once every 3 months, or within 4 weeks of the MHTP or PAMP being prepared, unless there are exceptional circumstances. An exceptional circumstance is when a patient has had a significant change in their mental health condition. In this case, to support their care, a GP should review the MHTP or PAMP at least once per course of treatment. Typically, a patient will not need more than 2 reviews in a calendar year.
From 1 November 2025, mental health treatment plan reviews and referrals will be undertaken using time-tiered (general) attendance items. This means a patient can receive a Medicare benefit based on the length of time they spend with the GP, and enables them to receive treatment for both their physical and mental health needs in the one appointment.
Do you have questions or feedback about the 1 November 2025 Better Access Changes? Don't hesitate to reach out to the GPMHSC at gpmhsc@racgp.org.au and we will do our best to answer your questions.